To evaluate the condition of bones and joints, X-ray radiography is usually performed—a method familiar to many people. However, the diagnostic capabilities of this method are limited. Moreover, its radiation load allows investigating only one area. If, for example, there is suspicion of an oncological process, another method is used—scintigraphy. It allows scanning all the bones and joints of the human skeleton and provides more accurate and detailed information.
In what cases, besides suspicion of cancer, is scintigraphy prescribed? How is it conducted? Is it harmful? Oleg Baranovsky, head of the isotope laboratory at the RCMC, explains.

— What is osteoscintigraphy?
— This method allows obtaining information about processes occurring in the skeletal system or that may occur with various diseases.
Scintigraphic examination of the skeletal system is widely used: it accounts for 50–60% of all diagnostic procedures in isotope diagnostics.
One of the main directions is the search for oncological transformations, that is, tumors, both malignant and benign. Therefore, the isotope laboratory is usually located in oncological institutions.
Any isotope examination, including osteoscintigraphy, involves the introduction of a special contrast agent - a radioactive label - into the body. It accumulates in one organ or system, and then scanning or detecting devices visualize and record it with specific properties and characteristics.
Osteoscintigraphy allows evaluating the distribution of this preparation in the bony structures of the human body and even joint segments several hours after the introduction of a special salt labeled with a technetium isotope.

Typically, it is the accumulation activity of this medication that corresponds to the pathological processes occurring in the bone tissue. Contrast selectively accumulates in these areas. Upon reaching certain concentrations, it is examined how non-physiological this is and what it can be attributed to.
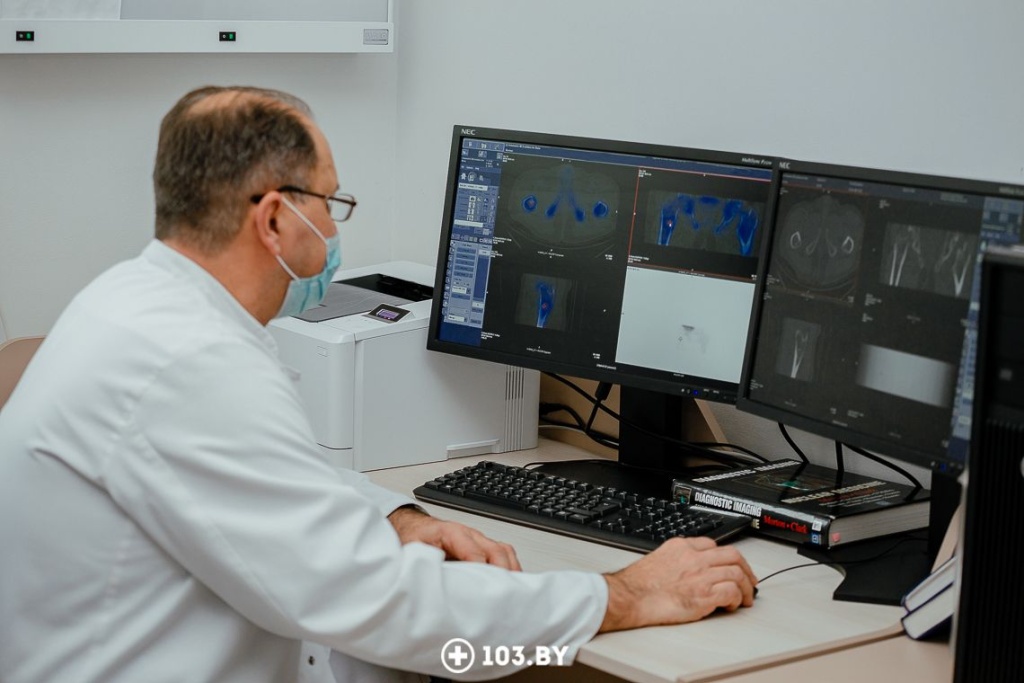
The machine used to examine the patient is, in essence, very similar to a conventional X-ray computed tomography machine, but operates differently.
— What distinguishes this tomograph from an X-ray one?
— An X-ray machine directly irradiates the person and, accordingly, captures a series of images on the opposite side based on the passage of X-ray beams.
The tomograph we use in nuclear medicine gathers information. In this case, the patient becomes a source of ionizing radiation. Rays emanate from the patient (in this case, from their bone tissue), which are concentrated and detected by detectors.

— Sounds scary... Is it harmful?
— I love this question. This radiopharmaceutical is diagnostic, it targets technetium-99, which has a half-life of only 6 hours. Of course, it is completely eliminated from the human body later — through the urinary system and gastrointestinal tract, but nonetheless.
The radiation exposure that a person receives during a flight, for example, to Turkey or Egypt and back, is practically comparable to the radiation exposure during this examination. The thing is, the plane typically flies at an altitude of 9 to 12 kilometers, which is already direct exposure to cosmic radiation.
The harm from applying any interventions to the human body should be compensated by the significance of the result. So, the information obtained about bone structures through osteoscintigraphy is quite significant.
Let's provide a clear example. Women with breast disease in the vast majority undergo osteoscintigraphy to assess possible changes in the skeletal system associated with the breast. This immediately changes the treatment strategy, the order, etc.
Osteoscintigraphy can detect secondary lesions from breast disease 2-5 months earlier, and sometimes even 1 year earlier than the usual radiographic method. And timely diagnosis of these lesions determines the timing of treatment, its effectiveness, and quality of life.

— In what other cases is osteoscintigraphy prescribed?
— When it is necessary to differentiate benign tumors from malignant bone tumors. Then a multi-phase scanning is used in several stages, sometimes with the repetition of certain actions. However, the results are almost comparable to histological results.
To assess the number of affected joints, their location, and the activity of changes in them. This helps rheumatologists to choose one or another tactic and sometimes change the treatment strategy, assess the functional activity of the lesion in systemic processes.
To assess the functional activity of spondylodiscitis processes — a fairly common pathology in the spine.
For tracking recovery dynamics after fractures. We are accustomed to this being mostly done through X-ray imaging. However, they can be quite limited when the patient has plaster casts, bandages, which partially shield and do not allow the full use of X-rays. Bone scintigraphy can be used without removing the casts.
To assess the stability or instability of endoprostheses, to determine the presence of inflammations, which often occur and require removal of the endoprosthesis, treatment of inflammatory reactions, installation of new endoprostheses.
For the purpose of assessing the functional activity of osteomyelitis – purulent inflammation of the bone marrow.
To clarify changes and possible genesis in bone structures, identified by other diagnostic methods (MRI, CT, radiography, etc.).
In cases of unexplained, unrelated pains, for example, in the back or in any limb.
For comprehensive assessment of fractures after trauma. After an impact and impairment of limb function or a fall from a height, a physician may prescribe X-ray imaging of the painful area, CT scans to evaluate soft tissues and the skeletal system. But combined and multiple traumas, damage to bone structures have not been ruled out. And their presence is practically impossible to detect using these methods.
There have been numerous cases where fractures were detected through bone scintigraphy that were not identified by X-ray methods, as only one area was examined. After all, you can't examine the entire skeleton with an X-ray – it's a significant radiation load. And with bone scintigraphy, this can be done objectively and simultaneously.
— How does the procedure go and how should one prepare for it?
— No special preparation is required. The only recommendation is to increase fluid intake 30-40 minutes after the administration of the medication. To do this, we ask the patient to bring along the beverages they prefer and as much as they can consume. The recommended fluid volume is up to 1 liter.
So, after consultation with the doctor, taking the medical history, and filling out the questionnaire, the patient signs the agreement. After that, the radiopharmaceutical is administered intravenously. During the interval between the injection and the scan in the tomograph, which typically takes 2-2.5 hours (although in certain cases, delayed scanning may be required: the following day), the patient stays in a special waiting room and gradually consumes their beverages - approximately a glass every 30-40 minutes. This allows for a clearer differentiation between soft tissue and bone structures and, most importantly, stimulates bladder emptying. And our active substance is primarily excreted through urine. Frequent voiding reduces the radiation dose to the bladder wall.
After 2-2.5 hours following the administration of the medication, the patient is invited for a tomographic scan. The examination lasts approximately 20 minutes. Only if there is a need for clarification of certain areas, additional scanning is conducted. Typically, this takes about 15-17 minutes. So, in total, a comprehensive spectrum of information can be obtained within 40 minutes.
One area is not examined during osteoscintigraphy. Due to the administration of the radiopharmaceutical, it is deemed imperative and unacceptable to not obtain information from the entire skeleton. Additionally, when assessing the integrity of endoprostheses (orthopedic surgeons often refer patients for osteoscintigraphy for this purpose), it is necessary to ensure that there are no infections present in other bone structures.

— What are the contraindications?
— Pregnancy is the only objective contraindication. In such cases, an alternative is chosen.
Following osteoscintigraphy, recommendations are given: we ask all patients in the coming days to avoid contact with pregnant women and children under 3 years old, as well as to empty the bladder and bowels more frequently to reduce radiation exposure.
—Is this an expensive procedure?
— The consumables, technetium-99 and special salt, are not very expensive. The price depends on the machine used for the procedure.
Currently, the most advanced machine is the gamma camera (or gamma tomograph) with semiconductor detectors. This provides higher accuracy and clearer differentiation of lesions from noise. Consequently, the specificity increases, and the reliability of the result sharply improves. Additionally, it allows for reducing the radioisotope dose for each patient, thus decreasing radiation exposure while maintaining or even improving the quality of results compared to other tomographs.
Moreover, this tomograph is combined with an X-ray computed tomograph. There are only four of such machines in the country, but only one with semiconductor detectors.
Even with this advanced technology, the procedure remains accessible, not more expensive than the regular cost of MRI or CT without contrast.
— How often can bone scintigraphy be performed?
— The frequency is determined based on the tasks at hand. Regarding its oncological relevance, despite obtaining sufficiently precise information, it cannot be said unequivocally that one conclusion or another can be drawn. Sometimes it is necessary to conduct the examination dynamically. To exclude or confirm secondary lesions, the examination is repeated in a month to a month and a half.
For non-oncological diseases (rheumatological, neurosurgical, and other processes), repeat examinations are possible no earlier than three months, usually after six months.
— Can this examination be done without clear indications, 'for preventive purposes'?
— This is not an ultrasound examination or magnetic resonance imaging. Anything involving exposure to ionizing radiation sources, in Belarus and throughout Europe, is not provided solely based on the patient's desire. A doctor's recommendation is necessary.
Interviewed by:Kristina Holoviychyk
Photo: Anna Zankovich
103.by