Ultrasound (US), magnetic resonance imaging (MRI), computed tomography (CT) - we all know these examinations, no need to decipher them. But what does this complex word on the prescription sheet mean - 'en-do-so-no-gra-phy'? Maybe it's not necessary to undergo it?
In reality, it is a quite serious examination with strict indications. Therefore, if you have been prescribed endosonography, it means that the doctor needs more detailed information about your gastrointestinal tract to establish an accurate diagnosis. Although this technology has both diagnostic and therapeutic capabilities... But let's take it step by step.
Journalist 103.by interviewed Tatiana Maevskaya, the head of the Endoscopy Department at the Republicanl Clinical Medical Center.

What is the purpose of this procedure?
— Endosonography is not a primary examination. Suppose you have undergone gastroscopy and a submucosal gastric lesion was found. Or on ultrasound, MRI, CT scans, some formations were detected in the pancreaticobiliary area, or there is suspicion regarding them... In such cases, endosonography is prescribed to refine the diagnosis.
This is an endoscopic technique performed using a special flexible instrument with an ultrasound probe at the tip.
Let me explain in more detail why a doctor may prescribe endosonography.
1. For the differential diagnosis of submucosal or non-epithelial gastrointestinal tract formations.
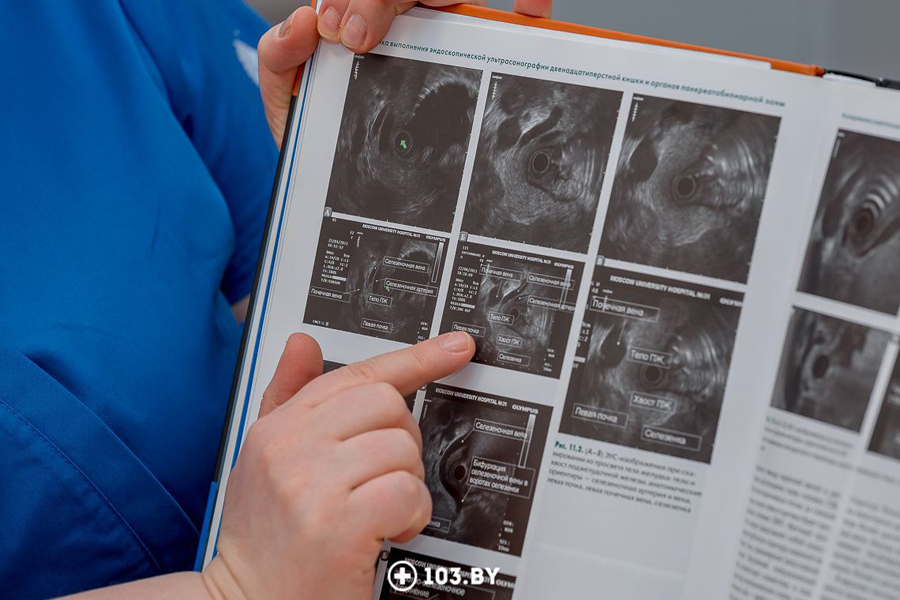
During a regular endoscopy, we can only see the presence of a formation, for example, oval-shaped, located beneath the mucous membrane. However, we cannot determine the nature of the formation. This is where endosonography comes into play.The instrument with an ultrasound probe is inserted and placed against the formation for scanning. This allows us to:
- Determine the size, structure, and originating layer of the formation;
- Differentiate between structures. Often, adjacent organs or formations from other organs may compress the gastric wall, making it impossible to accurately determine if it is an intramural formation or an extrinsic compression. Endosonography clearly shows this.
2. For determining the depth of invasion of gastrointestinal tract tumors, their local spread, and the presence of lymph node metastasis.
This is important when the tumor is in the early stages, and endoscopic removal is possible. In such cases, endosonography is performed to assess the depth of tumor invasion within the wall and to determine if it can be removed endoscopically.3. For the diagnosis of pancreaticobiliary diseases, pancreatic disorders, and major duodenal papilla conditions.
In other words, the technique allows for scanning specific points of the stomach and duodenum to:
- Clearly visualize the pancreas, liver, bile ducts, and pancreatic ducts, and detect focal formations, as well as inflammatory diseases;
- Conduct a differential diagnosis of cystic formations in the pancreas and solid formations in the pancreas;
- Perform fine-needle aspiration of cystic formations or fine-needle biopsy of solid formations in the pancreas and pancreaticobiliary area when necessary (this refers to therapeutic endosonography) to confirm the diagnosis.
4. For the differential diagnosis of thickened gastric folds (distinguishing between inflammatory and neoplastic processes).
5. For performing fine-needle biopsies of submucosal gastric formations.
6. Interventional techniques are currently being developed using endosonography, including:
- Drainage of pancreatic cysts;
- Administration of medications as indicated;
- Celiac plexus neurolysis
In addition to diagnosis, today therapeutic procedures can also be performed using endosonography. This is a rapidly developing field.
Endosonography is a significant examination conducted based on the doctor's recommendation. Consultation with an endoscopist is also necessary to evaluate indications and risks, and determine whether the procedure will be performed on an outpatient or inpatient basis.
Endosonography should not be performed "just in case."
How is the examination conducted? Is it lengthy? Can it be done under anesthesia?
— Usually, the procedure is performed under intravenous anesthesia to ensure maximum comfort for the person. To obtain clear visualization, it is necessary to precisely position the ultrasound probe against specific areas of the gastrointestinal wall and generate endosonographic images from specific angles. For this reason, the patient needs to lie still.
However, anesthesia is not as essential when performing rectal endosonography compared to esophageal, gastric, or duodenal endosonography, as it is not painful and there is no gag reflex.
The diagnostic procedure takes between 20 to 40 minutes depending on the objectives and is performed on an outpatient basis.
The examination is conducted similarly to a regular gastroscopy: an apparatus with an ultrasound probe is inserted into the esophagus, stomach, and duodenum. Depending on the purpose of the examination, the ultrasound probe is placed against the gastrointestinal wall at a standard point, resulting in both ultrasound and endoscopic images.
After the examination, the patient should be monitored in the recovery room for 2 hours. In most cases, this is sufficient as we have simply assessed the condition of the organs, performed submucosal ultrasound imaging, evaluated the pancreatobiliary zone, or examined the gastric wall.
If everything is normal, the patient can then go home. However, if intravenous anesthesia was used, driving a vehicle on the same day is not allowed, and it is advisable to limit physical exertion. It is recommended to consume light food such as broth or porridge 2 hours after the procedure to avoid burdening the body.
Therapeutic procedures (such as puncture or interventional interventions) may last up to an hour. However, this depends on the specific pathology and the amount of material required, such as during verification.
In such cases, the patient is hospitalized for one day. After the procedure, they are returned to the surgical department for observation. Operative endosonography carries certain risks, so it is necessary to monitor the patient.
Two hours after therapeutic endosonography, the patient is allowed to drink water but should refrain from eating.
If everything goes well, the patient is discharged the following day and can resume their normal life.

Can there be complications?
— Like with all endoscopic examinations, there is a risk of complications during endosonography. It is minimal, but it does exist.
Complications that can occur during any endoscopic examination include:
- Cardiovascular complications;
- Allergic reactions to medications;
- Anesthesia-related complications.
Now, let's talk about possible complications specific to endosonography.
- Perforation (a through-and-through injury) of the organ wall (the percentage is small, ranging from 0 to 0.4%). It usually occurs in areas of bends in the pharynx or in the area of the upper duodenal bend due to the fact that the instrument has a more rigid end compared to a gastroscope. If there are any anatomical peculiarities in the patient, there is a risk of injury. Therefore, as we have already mentioned, the procedure is performed strictly based on indications — only when it is necessary
- Bleeding (the probability is also low, ranging from 0.3 to 1%). It usually occurs during therapeutic endosonography when a fine needle puncture is performed.
- Development of acute pancreatitis and infectious inflammatory complications are also possible side effects specifically associated with therapeutic endosonography.

Who should not undergo this procedure?
— Contraindications for all endoscopic examinations include:
- General severe condition of the patient;
- Acute myocardial infarction;
- Acute cerebral circulation insufficiency;
- Severe cardiovascular or respiratory insufficiency.
It should be understood that the risks of the procedure are assessed in relation to the benefits of its performance. The decision is ultimately made by the attending clinician and the endoscopist.
Limitations to the procedure may include anatomical features such as narrowing of the digestive tract organs, scar or tumor strictures, or the presence of a diverticulum in the esophagus (like a pocket).
Therefore, prior to performing an endosonography, it is usually necessary to perform a routine esophagogastroduodenoscopy (gastroscopy) to determine if there are any obstacles for the passage of the device.

How to prepare for an endosonography?
— Endosonography of the upper gastrointestinal tract is performed on an empty stomach, so food intake should be avoided for 12 hours prior to the procedure, and fluid intake should be avoided for 6 hours. Typically, the patient does not eat anything after 6:00 PM and it is advisable not to drink anything after 10:00 PM.
If endosonography of the large intestine is being conducted, preparation is similar to that of a colonoscopy: the use of an enema or bowel cleansing medications is necessary. If the procedure is performed under anesthesia, it is also done on an empty stomach.
Interviewed by: Kristina Holovyichuk
Photo by: Anna Zankovich