Vertebral disc hernia (spinal disc herniation) is a displacement of nucleus pulposus of the vertebral disc accompanied by a rupture of the fibrous ring which results in the compression of spinal roots, vessels and the spinal cord.
Microfractures of the fibrous ring and penetration of receptors through its posterior areas are significant pathogenetic factors of discogenic pains.
INDICATIONS FOR SURGICAL INTERVENTION
- Discogenic pain syndrome is caused by the protrusion, or hernia, of the disk which occupies no more than 1/3 of the spinal canal;
- indicators of degenerative changes of the disk (increased intra-disk pressure, partial dehydration, internal ruptures and micro-fractures of the fibrous disk);
- local discogenic pain syndrome at the lumbar part of the spine in cases when conservative therapy did not show effect over a period exceeding three months;
- discogenic radicular pain syndrome.
SURGICAL TREATMENT OF VERTEBRAL DISC HERNIA AT THE RCMC
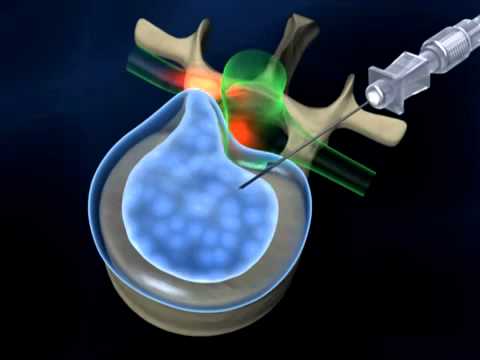
State Institution “RCMC” is the only Center in the Republic of Belarus where two modern minimally invasive interventions are performed for the treatment of acute and chronic pain syndrome in degenerative diseases of the spine, radiculopathy caused by intervertebral hernias. Minimally invasive surgery does not require deep anesthesia and large surgical skin incisions. Transcutaneous (percutaneous) puncture radio wave nucleoannuloplasty is performed using the DISK-FX system and cold plasma nucleoplasty using modern high-tech equipment.
Benefits of treating spinal diseases with nucleoplasty:
- no age restrictions;
- maximum accuracy (the operation is performed under X-ray navigation (control);
- minimum duration (the duration of the operation is short, about 20-30 minutes. The operation is performed in a hospital);
- minimal invasiveness (percutaneous insertion of the electrode, easily and precisely controlled volume of tissue removal);
- safety (the procedure is performed under intravenous anesthesia on spontaneous breathing, constant x-ray control accurately shows the position of the electrode in the intervertebral disc, there is no thermal damage to the treated tissue);
- efficiency (there is a complete decompression of the spinal root, the pain syndrome is stopped and the conduction disturbance in the nerve roots is eliminated, the functional properties of the intervertebral disc are restored, the defects of the fibrous ring are eliminated). The effectiveness of these interventions is 80-90%;
- minimal side effects and complications;
- long-term hospitalization is not required (the duration of hospitalization is determined by a specialist doctor individually, taking into account the protocols of management and instructions. Usually it takes 1-2 days);
- short recovery period. (the postoperative period does not require long-term rehabilitation and significant restrictions on physical activity).
CONTRAINDICATIONS
- Pronounced degenerative changes of the spinal disk (the height of the disk is reduced by more than 1/2; considerable dehydration of the disk);
- presence of a hernia which occupies more than 1/3 of the spinal canal; sequestered hernia;
- sequestered hernia;
- pronounced degenerative stenosis of the spinal canal accompanied by neurovascular compression phenomena;
- evidence of compression of spinal roots of two to three adjacent spinal bones;
- worsening neurological symptoms (muscular weakness, paresthesia, indicators of palsy or plegia);
- spondylolisthesis;
- segmental spinal instability in the area of the affected disk;
- traumatic injury of the spinal cord;
- presence of a tumor;
- occurrence of a local or generalized infection;
- spinal deformity;
- presence of spondylolysis;
- previous intervention on a spinal disk at the area of the planned intra-disc procedure.
PREPARATION FOR SURGERY INTERVENTION
In order to increase the effectiveness of the manipulations, it is necessary to determine clear indications and contraindications.
To determine the indications and contraindications for performing one of the indicated methods of treatment of intervertebral hernias and associated pain syndromes, as well as choosing the most optimal one, it is necessary to consult a specialist neurologist and neurosurgeon of our Center.
Consultations by specialist doctors are held in room G207 (see schedule information below).
Required examinations and documents for consultation
- An extract from the outpatient card at the place of residence, epicrisis of previous inpatient treatment (if any);
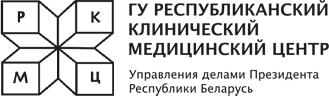
- CD-disc MRI of the spine with transcript;
- The passport
Hospitalization
Documents for hospitalization:
- extract from the outpatient card at the place of residence, epicrisis of previous inpatient treatment (if any), chest x-ray or fluorography (description with the seal of the medical institution, the limitation period is not more than one year)
- referral from a neurologist or neurosurgeon of the Center received during a consultation
- the result of a negative PCR test for covid infection, shelf life no more than 72 hours
- contract for the provision of paid services with a receipt for payment
On the day of hospitalization, an agreement for the provision of paid services is concluded at the register of paid services. You can pay the bill at the cash desk of the RKMC or through ERIP.
The cost of these manipulations is indicated in the price list on the Center's website.
Preoperative examination::- clinical blood test
- blood test for the presence of HBS antigen, anti-HCV
- biochemical blood test: ALT, AST, total protein, total bilirubin, urea, potassium, sodium, glucose, coagulogram-prothrombin, fibrinogen, INR blood type and Rh factor
- urinalysis
- ECG
- magnetic resonance imaging (MRI) of the spine for the planned operation
Этапы:
- The patient arrives at the clinic (the time and day of hospitalization are indicated in the referral), having the necessary documents with him (see above).
- Food and liquid intake is discussed individually with the doctor, with the exception of the usual medication, in the presence of concomitant diseases.
- After completing the documents and placing in the ward, conducting the necessary examination (see above), the attending physician, neurosurgeon and anesthetist assess the patient's condition and readiness for medical manipulation.
- The necessary preoperative preparation of the patient is carried out, the patient signs the “Informed voluntary consent for interventional treatment”, the patient is taken to the operating room.
- At the end of the manipulation, the patient returns to the ward. He is examined again by an anesthesiologist and a neurosurgeon in the ward. If the patient feels normal, in order to avoid complications and side effects, bed rest is recommended during the day.
- The attending physician discharges the patient. The terms of stay in the hospital and the terms of discharge from the hospital are determined by the attending physician according to the protocols of management. Upon discharge, the patient receives a discharge summary with recommendations for rehabilitation, a temporary disability certificate (if necessary).
HOW TO GET SURGICAL TREATMENT OF VERTEBRAL DISC HERNIA AT THE RCMC
- Call the Contact Center to make an appointment with a neurologist N.M. Chechik or, before hospitalization, contact neurosurgeon Kravets O.A.
Consultations by specialist doctors are held in room Г207 according to the following schedule:
Neurologist, Candidate of Medicine, associate professor Natalia Mikhailovna Chechik
Monday 10:30-12:00
Tuesday-Thursday 11:30-13:00
Neurosurgeon, the highest category, Oleg Aleksandrovich Kravets
Wednesday 17:00-20:00 - Come to the consultation on time
- Conclude a contract for the provision of paid services at the registry on the day of hospitalization.
- Pay the invoice at the cash desk of the RCMC or via ЕРИП (SSIS: Single Settlement and Information Space)
The information provided on the website is for informational purposes only and may be subject to change.